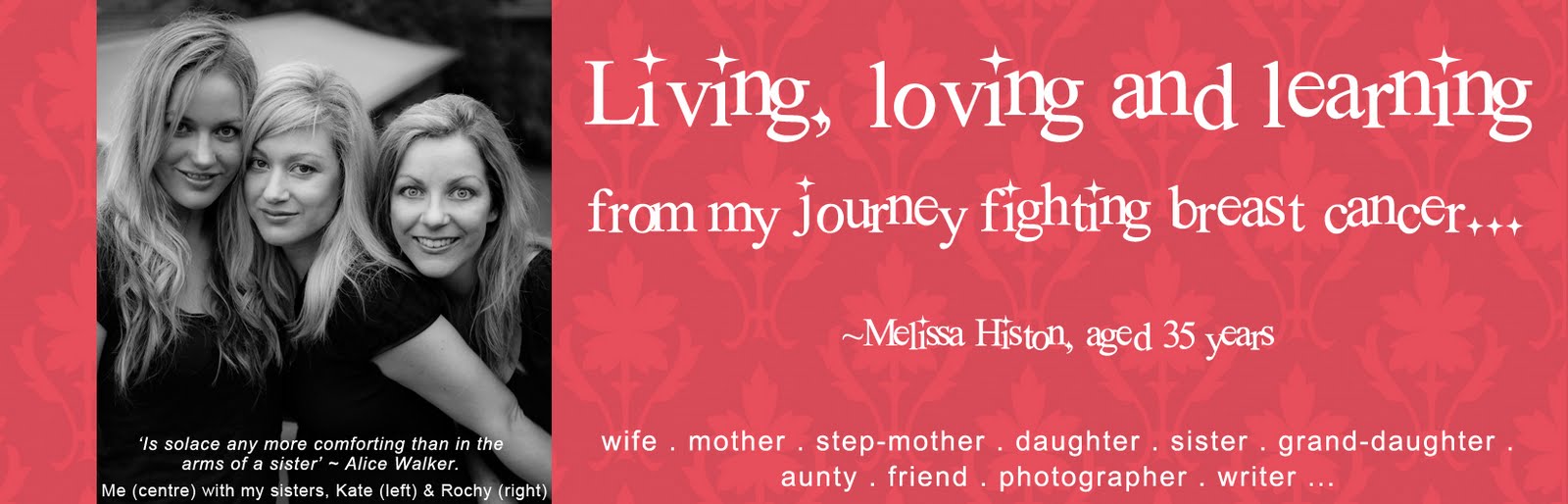
As I sat in my oncologist’s office after just having been told I needed chemotherapy, all I could think of was: how bad will the side effects be? And, what impact will this have on my family?
Until now, my only experience with cancer treatment has been Hollywood; i.e. what I have seen in the movies, which has pretty much been people with their head in a toilet. So my first endeavour was to find out how the chemo treatment would affect me.
I found that the oncologist’s booklets and internet were helpful listing general side effects that may occur for women who were treated with my particular chemotherapy drugs. (FYI, not all chemotherapy drugs are the same; even chemo drugs for breast cancer may differ from person-to-person, depending on type of breast cancer a person has). My particular chemotherapy drugs are TCH which stands for Taxotere, Carboplatin and Herceptin. These drugs kill off any fast dividing cells in a person’s body: both cancerous cells and any fast dividing healthy cells, such as hair cells and white blood cells.
My chemotherapy drugs are administered intravenously every third Monday. I find that Monday through to Wednesday of that first week, I don’t feel so bad. I am juiced up on steroids and anti-nausea tablets for these days so I feel a bit ‘wired’, I have trouble sleeping and feel hungry. It is from Wednesday evening of the first week that my side effects really take hold and last for about 1.5 weeks. After that, my white blood cell count builds up again and I feel more like my normal self.
Below are the physical side effects I have personally suffered:
Hair Loss
Chemotherapy drugs work by killing off any fast dividing cells in your body: both fast dividing healthy and cancer cells. Since hair cells are fast dividing, out comes your hair. My pubic hair began falling out two weeks after my first chemo session and fell out quickly, over a week or so (bonus: no more bikini waxes). The hair on my head began falling out a few days later. It came out more slowly and is not completely gone, but you can clearly see my scalp through the hair I have left. Funnily, I haven’t lost any other body hair and my eyebrows and eyelashes are still intact.
Nausea
If you have ever had morning sickness or a hang-over, you may be familiar with the all-consuming, terrible feeling of nausea. I liken it to a dark veil of sick draped over and wrapped around me that I can’t shrug off. It is worse in the morning: I wake feeling like death and dry-retching until I put some food in my belly and take an anti-nausea pill. Zofran wafers are great; they dissolve on my tongue (no need to worry about keeping down a tablet) and the relief is almost instantaneous. However, they are pretty expensive at about $50 for four wafers.
I find that the nausea worsens every couple of hours when my stomach is empty. If I have something to eat, it stops my stomach from churning and gives me a bit of relief until the next wave of nausea comes.
Thrush in my mouth
Within about two days after my chemo day, a thick, white blanket of thrush begins growing down my throat and on my tongue. Oral thrush feels just gross and makes eating and swallowing painful. At first, I didn’t realise it was thrush - never had it before – but once I figured it out, I purchased some Daktarin and Nilstat to kill it off, which did the trick.
After my second round of chemo, the thrush was back with much more ferocity and seemed to be dining on the Nilstat and spreading. So I went back to the chemist and bought more Daktarin: still not much of a change. My fabulous chemo nurse, Amy, suggested a prescription lozenge would help. This did the trick. Within a day, my thrush was gone! What a difference it made to my general feeling of wellness to have that foul thrush gone from my mouth and throat. Next round of chemo, I am going to hit that thrush hard with the lozenges before it takes hold (fingers crossed).
Aching bones
Okay, so not only do I look like a 90 year-old lady with my balding head, I have achy ol’ bones too. The aching is generally around my pelvis area and radiates up my spine and down my legs. When it gets too much, I take Panadeine Forte for relief (Nurofan Plus just doesn’t cut it).
Constipation
Yep, on top of everything else that that is going on, the cocktail of drugs I am taking – chemo drugs, steroids, pain killers, anti-nausea pills, mouth creams - clogs me up. Why does it always come back to poo? So prunes have been added to my diet (along with a laxative when it gets really bad)!
Loss of taste
People having chemo often report they get a horrid metallic taste in their mouth. I haven’t found that at all. Instead, for the first two weeks after chemo, most savoury foods taste very bland, sweet foods taste the same, alcohol tastes like kerosene, ice cream is fabulous!
The final week before my next hit of chemo my taste goes back to normal, so I chow down on all my favourite foods and my husband takes me out for some fantastic fine-dining fare! I have learned the importance of living for the moment and taking the time to savour my favourite things!
Sleeplessness
During week one of my chemotherapy cycle I have a lot of trouble sleeping at night. To avoid taking even more medications, I rely on my breathing exercises and meditation to relax and allow my body its healing time.
Fatigue
Okay, so I know that I said sleeplessness was a problem: but the silly contradiction is that fatigue is an even bigger problem during week one and two after chemo. I think I am having a good day and then ‘POW’, fatigue hits and I am floored and have to go to bed. I guess my body is telling me it needs some healing time so I have learned to just go with it when the fatigue hits.
INSIGHT
As I mentioned above, the worst of the side effects last about 1.5 weeks and then they start to improve and I have about a week of feeling like my happy, normal self. This whole process of experiencing physical pain while having my cancer treated has made me relish the time I feel good. I don’t take my wellness for granted…it is a gift! I have also learned to listen to my body and to provide what it needs. If I feel hungry – eat. If I feel tired or sick – rest. Eat foods that give me energy and nourishment: avoid foods that make me feel ill.
I am also learning to love my body for what it is. I love that it has been good to me for 35 years, working away, keeping my spirit alive. Yes, it has succumbed to cancer, but I believe that this whole experience has been a wake-up call to be kinder to myself; my spirit and my physical body. I know at the end of this year-long journey of treating my cancer, I will be dancing again!